Cold Agglutinin Disease (CAD)
Bay Biosciences provides high quality, clinical grade bio-specimens, cryogenically preserved sera (serum), plasma and peripheral blood mononuclear cells (PBMC) biofluid samples from patients diagnosed with Cold Agglutinin Disease (CAD).
The sera (serum), plasma and PBMC biofluid specimens are processed from patient’s peripheral whole-blood using customized collection and processing protocols. The cold agglutinin disease (CAD) bio-specimens are collected from unique patients diagnosed with cold agglutinin disease (CAD) disease and are provided to a valued pharmaceutical customer for research, diagnostics, discovery and drug development.
Detailed clinical data, cold agglutinin disease patients history, symptoms, complete blood count (CBC), elevated biomarker levels, genetic and metabolic information, histopathological findings, annotations associated with cold agglutinin disease (CAD) patient’s specimens is provided to a valued customer for research, development and drug discovery. The cold agglutinin disease (CAD) sera (serum), plasma and peripheral blood mononuclear cells (PBMC) biofluid are processed from patients peripheral whole-blood using customized collection and processing protocols.
Cold Agglutinin Disease (CAD) Overview
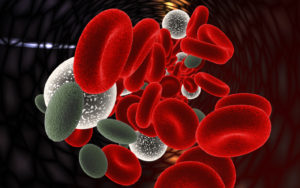
Cold agglutinin disease (CAD) is a rare acquired autoimmune disorder in which exposure to cold temperatures between 32 to 50 F (0 and 10 C) causes autoantibodies, also called cold agglutinins, to bind tightly to red blood cells (RBCs) and inducing their lysis (disintegration), resulting in anemia.
In cold agglutinin disease (CAD) autoantibodies bind to the erythrocyte membrane leading to premature erythrocyte destruction (hemolysis) characterize autoimmune hemolytic anemia. The presence of high concentrations of circulating cold sensitive antibodies, usually IgM and autoantibodies are active at temperatures below 30 °C (86 °F), directed against red blood cells, causing them to agglutinate and undergo lysis.
When cold agglutinin disease (CAD) patient’s blood is exposed to cold temperatures 32 °F (0 °C) to 50 °F (10 °C), certain proteins that normally attack bacteria (IgM antibodies) attach themselves to red blood cells and bind them together into clumps (agglutination). This eventually causes red blood cells to be prematurely destroyed (hemolysis) leading to anemia and other associated signs and symptoms. Cold agglutinin disease can be primary (unknown cause) or secondary, due to an underlying condition such as an infection, another autoimmune disease, or certain cancers. Treatment depends on many factors including the severity of the condition, the signs and symptoms present in each person, and the underlying cause.
Causes of Cold Agglutinin Disease (CAD)
Cold agglutinin disease (CAD) is caused by autoantibodies called cold agglutinins, which cling to RBCs at low temperatures. This causes the RBCs to clump together and prompts the immune system to destroy them, leading to severe depletion of RBCs in the blood and resulting in anemia.
CAD, which commonly affects adults who are of middle age and older, may manifest as a primary disease, in which the underlying mechanism is not known, or as a secondary disease caused by other underlying medical issues such as:
- Bacterial infections
- Viral infections
- Parasitic infections
- Other autoimmune diseases such as Systemic Lupus Erythematosus (SLE)
- Certain types of cancer
Signs and Symptoms Cold Agglutinin Disease (CAD)
Symptoms of cold agglutinin disease (CAD) are often triggered or made worse by cold temperatures or a viral infection. Therefore, symptoms generally are worse during winter months. Symptoms may arise suddenly leading to abrupt onset of severe anemia and hemoglobinuria or develop more gradually and insidiously in the background without patient’s realization. Most CAD patients have symptoms of hemolytic anemia (destruction of red blood cells, causing low levels of red blood cells), the number of symptoms and severity of symptoms may depend on how severe the anemia is.
Following are the common signs and symptoms of hemolytic anemia developed caused by Cold Agglutinin Disease (CAD):
- Cold hand and feet
- Chest pain
- Pain in the back and legs
- Fatigue
- Dark Urine
- Dizziness
- Headaches
- Jaundice
- Pale Skin
- Diarrhea
- Vomiting
Other symptoms of Cold Agglutinin Disease (CAD):
- Acrocyanosis: dark purple to grayish discoloration in the fingertips, nose, toes, and ears.
- Pain or discomfort swallowing cold foods and liquids
- Livido reticularis: Patchy, reticulated (spider web-like) vascular pattern on the skin with a red-blue or purple color.
- Raynaud’s Phenomenon: cold intolerance such as pain and a bluish color fingertips and toes.
- Skin ulceration or necrosis (in severe cases)
- Enlarged liver and spleen in some CAD cases
- Heart problems such as an irregular heartbeat (arrhythmias), heart murmur, enlarged heart which can lead to heart failure. These may occur because the heart has to work harder to make sure the body gets enough healthy red blood cells.
Diagnosis of Cold Agglutinin Disease (CAD)
Cold agglutinin disease (CAD) is suspected when patients show signs and symptoms typical of the CAD disease during cold temperatures. CAD also is suspected when there are unexplained reasons for hemolytic anemia or the observation of red blood cells (RBC) clumping in a cooled blood collection tube or a blood smear.
Following are several diagnostic tests performed to confirm Cold agglutinin disease (CAD):
- Blood tests such as a complete blood count (CBC) to detect anemia, the estimation of hemoglobin levels to analyze the extent of anemia, tests to identify and quantify reticulocytes, which are immature red blood cells that are normally not present in the blood, but are found in conditions of hemolytic anemia while the body tries to compensate for low RBC counts.
- A blood smear that can reveal the abnormal clumping (agglutination) of the RBCs.
- Biochemical tests on blood samples to identify the levels of the lactate dehydrogenase (LDH) enzyme, haptoglobin protein, and the liver metabolite, bilirubin, which is produced by the breakdown of hemoglobin. In general, hemolysis is accompanied by a significant increase in LDH
and bilirubin levels and a decrease in haptoglobin levels. - A physical examination that can detect hepatosplenomegaly.
- Direct Coombs test or antiglobulin that can detect the presence of autoantibodies immunoglobulin M (IgM) or cold agglutinins or the complement proteins that are attached to the surface of the RBCs.
Treatment of Cold Agglutinin Disease (CAD)
Cold agglutinin disease (CAD) patients whose disease symptoms are not severe, drug therapy is not required, and CAD can be resolved by avoiding exposure to cold, keeping warm, or moving to a warmer climate.
In more severe CAD cases, monotherapy with Rituximab, an antibody that selectively binds to and induces the destruction of immune cells called B-cells that produce the autoantibodies, can be used. This is effective in about 60% of cases. The response is generally observed within one to two months of treatment, and the effect of the treatment can last one to two years. However, Rituximab is now recommended as the first-line treatment of CAD.
Combined treatment with rituximab and fludarabine results in higher response rates (76% of cases) and longer periods of remissions (on average, 6.5 years). However, the combined treatment can have serious side effects. That is why it is recommended only when rituximab has not worked alone.
Rituximab combined with oral Cytoxan (cyclophosphamide), prednisone or other immunosuppressive medications may be used for cases of CAD that do not resolve with other treatments.
In more severe cases, plasma exchange or plasmapheresis may be performed to remove the IgM or cold agglutinin antibodies from the blood to reduce or alleviate disease symptoms. However, the effect of plasmapheresis is temporary because the B-cells that generate these antibodies are not removed by this procedure. It is useful to overcome acute hemolytic crisis and before surgery-requiring hypothermia.
Previously, corticosteroids treatment has been prescribed for CAD patients. However, patients usually require very high doses of corticosteroids to alleviate symptoms (at levels not considered safe). Hence, corticosteroid treatment is no longer recommended.
In extreme cases, a blood transfusion may be required. Care has to be taken to transfuse warm blood. Moreover, transfusion of blood products with high plasma content should be avoided because elevated levels of complement proteins can cause hemolysis, which exacerbates the condition.

Bay Biosciences is a global leader in providing researchers with high quality, clinical grade, fully characterized human tissue samples, bio-specimens and human bio-fluid collections from cancer (tumor) tissue, cancer serum, cancer plasma cancer PBMC and human tissue samples from most other therapeutic areas and diseases.
Bay Biosciences maintains and manages it’s own bio-repository, human tissue bank (biobank) consisting of thousands of diseased samples (specimens) and from normal healthy donors available in all formats and types. Our biobank procures and stores fully consented, deidentified and institutional review boards (IRB) approved human tissue samples and matched controls.
All our human human tissue collections, human specimens and human bio-fluids are provided with detailed samples associated patient’s clinical data. This critical patient’s clinical data includes information relating to their past and current disease, treatment history, lifestyle choices, biomarkers and genetic information. Patient’s data is extremely valuable for researchers and is used to help identify new effective treatments (drug discovery & development) in oncology, other therapeutic areas and diseases. This clinical information is critical to demonstrate their impact, monitor the safety of medicines, testing & diagnostics, and generate new knowledge about the causes of disease and illness.
Bay Biosciences banks wide variety of human tissue samples and biological samples including cryogenically preserved -80°C, fresh, fresh frozen tissue samples, tumor tissue samples, FFPE’s, tissue slides, with matching human bio-fluids, whole blood and blood derived products such as serum, plasma and PBMC’s.
Bay Biosciences is a global leader in collecting and providing human tissue samples according to the researchers specified requirements and customized, tailor made collection protocols. Please contact us anytime to discuss your special research projects and customized human tissue sample requirements.
Bay Biosciences provides human tissue samples (human specimens) from diseased and normal healthy donors; including peripheral whole-blood, amniotic fluid, bronchoalveolar lavage fluid (BAL), sputum, pleural effusion, cerebrospinal fluid (CSF), serum (sera), plasma, peripheral blood mononuclear cells (PBMC’s), saliva, Buffy coat, urine, stool samples, aqueous humor, vitreous humor, kidney stones, renal calculi, nephrolithiasis, urolithiasis and other bodily fluids from most diseases including cancer. We can also procure most human bio-specimens and can do special collections and requests of human samples that are difficult to find. All our human tissue samples are procured through IRB approved clinical protocols and procedures.
In addition to the standard processing protocols Bay Biosciences can also provide human plasma, serum, PBMC bio-fluid samples using custom processing protocols, you can buy donor specific sample collections in higher volumes and specified sample aliquoting from us. Bay Biosciences also provides human samples from normal healthy donors, volunteers, for controls and clinical research, contact us Now.
日本のお客様は、ベイバイオサイエンスジャパンBay Biosciences Japanまたはhttp://baybiosciences-jp.com/contact/までご連絡ください。


