Relapsing Polychondritis Specimens
Bay Biosciences provides high quality, clinical grade bio-samples, cryogenically preserved tissue, FFPE blocks, sera (serum), plasma and peripheral blood mononuclear cells (PBMC) biofluid specimens from patients diagnosed with Relapsing Polychondritis (RP) Disease.
The sera (serum), plasma and peripheral blood mononuclear cells (PBMC) biofluid samples are processed from patient’s peripheral whole-blood using customized collection and processing protocols.
The Relapsing Polychondritis (RP) Disease bio-specimens are collected from unique patients diagnosed with Relapsing Polychondritis (RP) Disease and are provided to a valued pharmaceutical customer for translational research, genomics, proteomics and biomarker research, drug discovery and development.
Relapsing Polychondritis (RP) Disease Overview
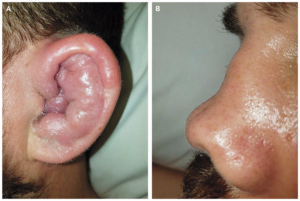
Relapsing Polychondritis (RP) is a rare degenerative disease characterized by recurrent inflammation of the cartilage and other tissue throughout the body. Cartilage is a tough but flexible tissue that covers the ends of bones at a joint, and gives shape and support to other parts of the body. Deterioration of the cartilage may affect any site of the body where cartilage is present. Ears, larynx and trachea (cartilaginous structures) may become “floppy,” and the bridge of the nose can collapse into a “saddle-nose” shape. The aortic heart valve may also be affected. Ear involvement is the most common feature, but a variety of other areas of the body may be affected, including the costal (rib) cartilage, eyes, nose, airways, heart, vascular (veins) system, skin, joints, kidney, and nervous system. The signs and symptoms vary from person to person depending on which parts of the body are affected. The exact underlying cause of Relapsing Polychondritis (RP) is unknown and it occurs most often in people in their 50s or 60s; however, scientists suspect that it is an autoimmune condition.
Relapsing Polychondritis (RP) Disease Symptoms
Relapsing Polychondritis (RP) is characterized by recurrent inflammation of cartilage (the tough but flexible tissue that covers the ends of bones at a joint) and other tissues throughout the body. The features of the condition and the severity of symptoms vary significantly from person to person, but may include:
- Ear- The ears are the most commonly affected body part. Symptoms include a sudden onset of pain, swelling, and tenderness of the cartilage of one or both ears. The pinna
usually loses firmness and becomes floppy; hearing impairment may also occur. Inflammation of the inner ear may also cause nausea, vomiting, dizziness, and/or ataxia. - Joint Pain– The second most common finding in Relapsing Polychondritis (RP) disease is joint pain with or without arthritis.
- Eye- Affected people may experience episcleritis, uveitis and/or scleritis. Scleritis may lead to a bluish or dark discoloration of the sclera (white of the eye) and may even be associated with vision loss in severe cases. Proptosis (bulging out of one or both eye balls) may also be a symptom of Relapsing Polychondritis (RP) disease.
- Nose- Nasal cartilage inflammation may lead to stuffiness, crusting, rhinorrhea, epistaxis (nose bleeds), compromised sense of smell and/or saddle nose deformity (a condition where the nose is weakened and thus “saddled” in the middle).
- Airways- In Relapsing Polychondritis (RP) disease inflammation may affect the larynx, trachea (windpipe), and bronchi (tubes that branch off the trachea and carry air to the lungs). Airway involvement may lead to a cough, wheezing, hoarseness and recurrent infections. It can become life-threatening if not properly diagnosed and managed.
In approximately one third of the patients affected by Relapsing Polychondritis (RP) disease is associated with other medical problems. Conditions reportedly associated with RP include hematological disease (including Hodgkin’s Lymphoma and myelodysplastic syndromes); gastrointestinal disorders (including Crohn’s disease and Ulcerative Colitis); endocrine diseases (including diabetes mellitus type -1 and thyroid disorders) and others. Episodes of Relapsing Polychondritis (RP) disease may last a few days or weeks and typically resolve with or without treatment. However, it is generally progressive, and many people have persistent symptoms in between flares.

Causes of Relapsing Polychondritis (RP) Disease
The exact underlying cause of Relapsing Polychondritis (RP) is unknown. However, scientists suspect that it is an autoimmune disease. It it thought that Relapsing Polychondritis (RP) occurs when the body’s immune system mistakenly attacks its own cartilage and other tissues. In general, autoimmune conditions are complex traits that are associated with the effects of multiple genes in combination with lifestyle and environmental factors.
There is also evidence to suggest that some people may be born with a genetic susceptibility to Relapsing Polychondritis (RP) disease. Studies have found that people with RP are roughly twice as likely as those without this condition to carry a certain genetic allele called HLA-DR4. “HLA” stands for Human Leukocyte Antigen, which is an important part of our immune system and plays a role in resistance and predisposition (risk) to disease. However, HLA genes are not solely responsible for specific diseases but instead may simply contribute along with other genetic or environmental factors to disease risk. Thus, many people with HLA-DR4 will never develop Polychondritis.
Relapsing Polychondritis (RP disease) is not passed through families in a clear-cut fashion. Most people with Relapsing Polychondritis do not have affected relatives. Like many other autoimmune conditions, RP is likely a multifactorial condition which is associated with the effects of multiple genes in combination with lifestyle and environmental factors. In general, having a first degree relative (for example a parent, child, or sibling) with an autoimmune condition may increase the personal risk for developing an autoimmune condition. Unfortunately, no specific risk estimates are available for Relapsing Polychondritis (RP) disease.
Relapsing Polychondritis (RP) Disease Diagnosis
There are no specific tests available for for Relapsing Polychondritis (RP) disease. A diagnosis is, therefore, generally based on the presence of characteristics and signs and symptoms. In some cases, a biopsy affected tissue may be necessary to support the diagnosis. For example, people may be diagnosed as having Relapsing Polychondritis (RP) disease, if they have three or more of the following features:
- Inflammation of the cartilage of both ears
- Seronegative (negative for Rheumatoid Factor) polyarthritis (arthritis that involves 5 or more joints simultaneously)
- Inflammation of the cartilage of the nose
- Eye inflammation (Conjunctivitis, Episcleritis, scleritis, and /or uveitis)
- Inflammation of the cartilage of the airway
- Vestibular Dysfunction (i.e. Vertigo, hearing loss, Tinnitus)

Relapsing Polychondritis (RP) Disease Treatment
The primary goals of treatment for patients with Relapsing Polychondritis (RP) disease are to relieve present symptoms and to preserve the structure of the affected cartilage. The main treatment for RP is corticosteroid therapy with prednisone to decrease the severity, frequency and duration of relapses. Higher doses are generally given during flares, while lower doses can typically be prescribed during periods of remission. Patients who develop severe heart or respiratory complications may require surgery.
Relapsing Polychondritis (RP) Disease Prognosis
The long-term outlook (prognosis) for patients with Relapsing Polychondritis (RP) disease varies from person to person. In general, RP is a chronic and progressive (worsening overtime) condition. Some form of disability is common in the later stages of Relapsing Polychondritis (RP) disease; these may include Visual Impairment, Hearing Loss, Vestibular Dysfunction, and/or Cardiopulmonary (heart and lung) disease. Severe cases of Relapsing Polychondritis (RP) disease can be life-threatening. Respiratory complications (windpipe collapse and infections) are the most common cause of death followed by Cardiovascular (heart and blood vessel) involvement.

Detailed clinical data, MRI scan, elevated biomarker levels, genetic & metabolic information, pathology annotations associated with the Relapsing Polychondritis Disease patient’s specimens is provided to a valued customer for translational research, drug discover, development and research. The Relapsing Polychondritis Disease PBMC’s, sera and plasma samples are processed from patients peripheral whole-blood using customized processing protocols provided by the researcher.
Bay Biosciences is a global leader in providing researchers with high quality, clinical grade, fully characterized human tissue samples, bio-specimens and human bio-fluid collections from cancer (tumor) tissue, cancer sera (serum), cancer plasma, cancer PBMC and human tissue samples from most other therapeutic areas and diseases.
Bay Biosciences maintains and manages it’s own bio-repository, human tissue bank (biobank) consisting of thousands of diseased samples (specimens) and from normal healthy donors available in all formats and types. Our biobank procures and stores fully consented, deidentified and institutional review boards (IRB) approved human tissue samples and matched controls.
All our human human tissue collections, human specimens and human bio-fluids are provided with detailed samples associated patient’s clinical data. This critical patient’s clinical data includes information relating to their past and current disease, treatment history, lifestyle choices, biomarkers and genetic information. Patient’s data is extremely valuable for researchers and is used to help identify new effective treatments (drug discovery & development) in oncology, other therapeutic areas and diseases. This clinical information is critical to demonstrate their impact, monitor the safety of medicines, testing & diagnostics, and generate new knowledge about the causes of disease and illness.
Bay Biosciences banks wide variety of human tissue samples and biological samples including cryogenically preserved -80°C, fresh, fresh frozen tissue samples, tumor tissue samples, FFPE’s, tissue slides, with matching human bio-fluids, whole blood and blood derived products such as serum, plasma and PBMC’s.
Bay Biosciences is a global leader in collecting and providing human tissue samples according to the researchers specified requirements and customized, tailor made collection protocols. Please contact us anytime to discuss your special research projects and customized human tissue sample requirements.
Bay Biosciences provides human tissue samples (human specimens) from diseased and normal healthy donors; including peripheral whole-blood, amniotic fluid, bronchoalveolar lavage fluid (BAL), sputum, pleural effusion, cerebrospinal fluid (CSF), serum (sera), plasma, peripheral blood mononuclear cells (PBMC’s), saliva, Buffy coat, urine, stool samples, aqueous humor, vitreous humor, kidney stones, renal calculi, nephrolithiasis, urolithiasis and other bodily fluids from most diseases including cancer. We can also procure most human bio-specimens and can do special collections and requests of human samples that are difficult to find. All our human tissue samples are procured through IRB approved clinical protocols and procedures.
In addition to the standard processing protocols Bay Biosciences can also provide human plasma, serum, PBMC bio-fluid samples using custom processing protocols, you can buy donor specific sample collections in higher volumes and specified sample aliquoting from us. Bay Biosciences also provides human samples from normal healthy donors, volunteers, for controls and clinical research, contact us Now.
日本のお客様は、ベイバイオサイエンスジャパンBay Biosciences Japan またはhttp://baybiosciences-jp.com/contact/までご連絡ください。


