Bay Biosciences provides high-quality fresh frozen sera (serum), plasma, and peripheral blood mononuclear cells (PBMC) bio-fluids, from patients diagnosed with thrombotic thrombocytopenic purpura (TTP).
The sera (serum), plasma and PBMC biofluid specimens are processed from patient’s peripheral whole-blood using customized collection and processing protocols from thrombotic thrombocytopenic purpura (TTP).
Fresh frozen tissue and matched biofluid samples are collected from unique patients diagnosed with thrombotic thrombocytopenic purpura (TTP).
Bio-samples are provided to a valued pharmaceutical customer for research, diagnostics, discovery and drug development.

Thrombotic Thrombocytopenic Purpura (TTP) Overview
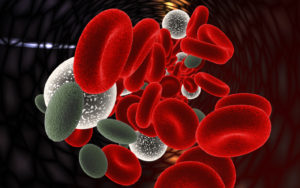
Thrombotic thrombocytopenic purpura (TTP) is a blood disorder that results in blood clots forming in small blood vessels circulating throughout the body. This results in a low platelet count, low red blood cells due to their breakdown and brain, heart and kidney dysfunction.
Too many of your blood’s platelets may also combine to form the clots. Your blood might then be unable to form clots when it needs to. For example, if you’re injured, you may be unable to stop bleeding.
Platelets are the blood cells that help to clot our blood when we are bleeding. Because the platelet count is low, these people are at risk for bleeding. Most patients also become anemic as a result of the TTP. Red blood cells are destroyed faster than the body can make new ones.
The exact prevalence of TTP is unknown. According to Stat Pearls, prevalence of thrombotic thrombocytopenic purpura (TTP) may range from 1 to 13 cases per million. and it varies by geographic location.
Thrombotic Thrombocytopenia Purpura (TTP) is a rare disorder of the blood coagulation system and is considered a serious medical emergency.
TTP is characterized into acquired (idiopathic) and congenital (inherited/familial), affecting more women patients than men with a peak incidence in patients in their forties.
This disease causes extensive clots (microscopic thromboses) to form in small blood vessels throughout the body (thrombotic microangiopathy).
TTP is one of the microangiopathic hemolytic anemias, and is characterized by the presence in the plasma of large von Willebrand Factor (VWF) strings. VWF is a large protein involved in blood clotting.
Most cases of TTP arise from lack of an enzyme known as ADAMTS13 gene, which is responsible for breaking down large strings of VWF into smaller units, which then reduces the small blood vessel clots. Often the ADAMTS 13 stops working because your body makes antibodies to it.
Types of Thrombotic Thrombocytopenic Purpura (TTP)
Cancer and organ transplantation-associated TTP
Among all TMA suspicion in patients with cancer, hematopoietic stem cell transplantation, or organ transplantation, those whose ADAMTS13 activity is undetectable at presentation are few.
These forms of TTP occur equally in men and women, have an older age of onset, are not the result of an immune-mediated ADAMTS13 deficiency, and portend a worse prognosis when compared with other forms of TTP.
Cancer and organ transplantation-associated TTP are poorly responsive to TPE. In addition, cancer may be either a known preexisting condition to TTP or discovered concomitantly.
Idiopathic TTP and TTP associated with another autoimmune disease
These TTP forms have 2 main common features underlining the strong autoimmune background of TTP: a female predominance (sex ratio ∼2.5 females to 1 male) and a high rate (∼90%) of positive ADAMTS13 autoantibodies during acute TTP events.
In addition, during follow-up, ∼10% of patients with idiopathic TTP develop other autoantibodies either isolated or associated with clinical symptoms of another autoimmune disease (mainly anti-dsDNA and SLE).
HIV-associated TTP
TTP can typically reveal a HIV infection that needs to be rapidly identified. HIV infection does not alter the usually favorable prognosis of TTP, and response to plasma therapy as well as remission and survival rates are comparable to those of patients with idiopathic TTP.
Such patients should therefore benefit from the usual measures in TTP management (eg, intensive and possibly prolonged plasma therapy with TPE), along with highly active antiretroviral therapy.
Obstetric TTP
Pregnancy-associated TTP mostly occurs during the second half of pregnancy. In the case of USS, TTP occurs as soon as the first pregnancy. In the acquired form of TTP, the first episode may occur during any pregnancy.
The rate of fetal loss reported remains high (∼40%), but studies are mainly retrospective and include a high proportion of women misdiagnosed and lately managed for TTP.
Signs and Symptoms of Thrombotic Thrombocytopenic Purpura (TTP)
In very serious TTP cases, a patient can have a stroke, a major internal bleeding or a coma can occur. Following are the common signs and symptoms of thrombotic thrombocytopenic purpura (TTP):
Skin Related Symptoms
- Bruises that are purplish in color and have no obvious cause. These marks, called purpura, are part of what gives this condition its name.
- Skin looks pale
- Tiny red of purple spots that look like a rash
- The skin may turn yellow, which is known as jaundice
Other Symptoms of TTP
Thrombotic thrombocytopenic purpura (TTP) patients may also have other following symptoms:
Causes of Thrombotic Thrombocytopenic Purpura (TTP)
There are two types of thrombotic thrombocytopenic purpura (TTP)
-
Acquired (idiopathic)
-
Congenital (inherited/familial)
Acquired TTP
In some cases, the body mistakenly produces proteins that interfere with the ADAMTS13 enzyme’s job. This is known as acquired TTP.
You can get acquired TTP in a various ways. You can develop it if you have HIV, for example. You can also develop it after certain medical procedures, such as a blood and marrow stem cell transplant and surgery.
In certain cases, TTP can develop during pregnancy or if you have cancer or an infection.
Some medications can also lead to the development of TTP. These include the following:
- Chemotherapy
- Medicines (including ticlopidine, clopidogrel, quinine, and cyclosporine A)
- Cyclosporine (Neoral, Sandimmune), which is an immunosuppressant drug
- Hormone therapy
- Estrogen, as used in birth control
- Hormone therapy
Diagnosis of Thrombotic Thrombocytopenic Purpura (TTP)
Your doctor may begin by performing a physical exam. This involves looking for any of the physical symptoms of the disease.
Diagnosing TTP usually requires multiple tests including blood tests. A diagnosis may be made based upon a thorough clinical evaluation, a detailed patient history and identification of characteristic findings.
The diagnosis is confirmed by the finding of severely deficient (<10%) ADAMTS13 gene activity and the presence of an anti-ADAMTS13 antibody in patients with iTTP.
An examination of the red blood cells (RBCs) under a microscope will reveal whether they have damage from TTP. They’ll also look for high levels of bilirubin, a substance that results from the breakdown of RBCs.
Your doctor will also check your blood for:
- Antibodies, which are proteins that interfere with the enzyme ADAMTS13
- A lack of ADAMTS13 enzyme activity, which causes TTP
- High creatinine levels, because TTP can cause kidney problems (which affects the kidneys’ ability to filter creatinine)
- Low platelet levels, because the increased clotting causes increased use of platelets
- The enzyme lactate dehydrogenase, which is released from tissue injured by blood clots that are caused by TTP
Treatment of Thrombotic Thrombocytopenic Purpura (TTP)
Doctors usually treat thrombotic thrombocytopenic purpura (TTP) by trying to return the patients blood clotting ability to normal. Plasma treatments are the most common way to treat TTP. Other treatments include medicines and surgery.
The treatment for thrombocytopenia can vary depending on how low a person’s platelet count becomes. If the platelet count falls within 100,000 – 150,000 per microliter of blood, the blood can still clot, meaning that the increase in the risk of bleeding is not significant.
Thrombotic thrombocytopenic purpura (TTP) can be fatal or cause lasting damage, such as brain damage or a stroke, if it’s not treated right away.
In most cases, TTP occurs suddenly and lasts for days or weeks, but it can go on for months.
Relapses (flareups) can occur in up to 60 percent of people who have acquired TTP. Flareups also occur in most people who have inherited TTP.
Plasma Therapy
Thrombotic thrombocytopenic purpura (TTP) causes platelets to clump together throughout the body, forming small blood clots. This effect lowers the platelet count.
The standard treatment for TTP is plasma exchange. During plasma exchange, a healthcare professional removes a patients plasma and replaces it with healthy blood plasma, which includes healthy platelets. This procedure works in a similar way to a blood transfusion and requires the insertion of an IV line into a vein.
Plasma is the liquid part of your blood. It carries blood cells, hormones, enzymes, and nutrients to your body.
TTP is treated with plasma therapy. This includes:
- Fresh frozen plasma for patients who have inherited TTP
- Plasma exchange for patients who have acquired TTP
Plasma therapy is started in the hospital as soon as TTP is diagnosed or suspected.
For inherited TTP, fresh frozen plasma is given through an intravenous (IV) line inserted into a vein. This is done to replace the missing or changed ADAMTS13 enzyme.
If plasma exchange isn’t available, you may be given fresh frozen plasma until it is available.
During plasma exchange, an IV needle or tube is placed in a vein in your arm to remove blood. The blood goes through a cell separator, which removes plasma from the whole-blood. The non-plasma part of the blood is saved, and donated plasma is added to it.
Then, the blood is put back into you through an IV line inserted into one of your blood vessels. The time required to complete the procedure varies, but it often takes about 2 hours.
Treatments of fresh frozen plasma or plasma exchange usually continue until your blood tests results and signs and symptoms improve. This can take days or weeks, depending on the patients condition. Usually the patient stay in the hospital while they recover.
Some patients who recover from TTP can have flareups. This can happen in the hospital or after they are discharged from the hospitals and go home. If you have a flareup, the doctors will restart plasma therapy.
Other Treatments
Other treatments are used if plasma therapy doesn’t work well or if flareups occur often.
For acquired TTP, medicines can slow or stop antibodies to the ADAMTS13 enzyme from forming. Medicines used to treat TTP include glucocorticoids, vincristine, rituximab, and cyclosporine A.
Sometimes surgery to remove the spleen (an organ in the abdomen) is needed. This is because cells in the spleen make the antibodies that block ADAMTS13 enzyme activity.
Surgery
In other cases, the patients spleen might need to be surgically removed. Removal of the spleen can help increase the platelet count.
A splenectomy involves removing the spleen, which is the organ that stores platelets, keeping them out of circulation. It is also the place where the body produces the antibodies that destroy platelets in cases of primary ITP.
About 50% to 70% of patients who choose this treatment recover from thrombocytopenia. However, predicting how well someone will respond can be difficult, and there is no way to know whether the surgery will work.
Surgery also carries some risks, such as bleeding and infection.
Risk Factors of Thrombotic Thrombocytopenic Purpura (TTP)
Thrombotic thrombocytopenic purpura is a rare disorder. Most cases of TTP are acquired. Acquired TTP mostly occurs in adults, but it can affect children. The condition occurs more often in women and in African Americans than in other ethnicities.
Inherited TTP mainly affects newborns and children. Most patients who have inherited TTP begin to have symptoms soon after birth. Some, however, don’t have symptoms until they’re adults.
It isn’t clear what triggers inherited and acquired TTP, but some factors may play a role. These factors may include:
- Some diseases and conditions, such as pregnancy, cancer, HIV, lupus, and infections
- Certain medical procedures, such as surgery and blood and marrow stem cell transplant
- Some medicines, such as chemotherapy, ticlopidine, clopidogrel, cyclosporine A, and hormone therapy and estrogens
- Quinine, which is a substance often found in tonic water and nutritional health products

Bay Biosciences is a global leader in providing researchers with high quality, clinical grade, fully characterized human tissue samples, bio-specimens and human bio-fluid collections.
Samples available are cancer (tumor) tissue, cancer serum, cancer plasma cancer PBMC and human tissue samples from most other therapeutic areas and diseases.
Bay Biosciences maintains and manages its own bio-repository, human tissue bank (biobank) consisting of thousands of diseased samples (specimens) and from normal healthy donors available in all formats and types.
Our biobank procures and stores fully consented, deidentified and institutional review boards (IRB) approved human tissue samples and matched controls.
All our human tissue collections, human specimens and human bio-fluids are provided with detailed samples associated patient’s clinical data.
This critical patient’s clinical data includes information relating to their past and current disease, treatment history, lifestyle choices, biomarkers and genetic information.
Patient’s data is extremely valuable for researchers and is used to help identify new effective treatments (drug discovery & development) in oncology, other therapeutic areas and diseases.
Bay Biosciences banks wide variety of human tissue samples and biological samples including cryogenically preserved at – 80°C.
Including fresh frozen tissue samples, tumor tissue samples, FFPE’s, tissue slides, with matching human bio-fluids, whole blood and blood derived products such as serum, plasma and PBMC’s.
Bay Biosciences is a global leader in collecting and providing human tissue samples according to the researchers specified requirements and customized, tailor-made collection protocols.
Please contact us anytime to discuss your special research projects and customized human tissue sample requirements.
Bay Biosciences provides human tissue samples (human specimens) from diseased and normal healthy donors which includes:
- Peripheral whole-blood,
- Amniotic fluid
- Bronchoalveolar lavage fluid (BAL)
- Sputum
- Pleural effusion
- Cerebrospinal fluid (CSF)
- Serum (sera)
- Plasma
- Peripheral blood mononuclear cells (PBMC’s)
- Saliva
- Buffy coat
- Urine
- Stool samples
- Aqueous humor
- Vitreous humor
- Kidney stones (renal calculi)
- Other bodily fluids from most diseases including cancer.
We can also procure most human bio-specimens and can-do special collections and requests of human samples that are difficult to find. All our human tissue samples are procured through IRB approved clinical protocols and procedures.
In addition to the standard processing protocols Bay Biosciences can also provide human plasma, serum, PBMC bio-fluid samples using custom processing protocols, you can buy donor specific sample collections in higher volumes and specified sample aliquots from us.
Bay Biosciences also provides human samples from normal healthy donors, volunteers, for controls and clinical research, contact us Now.
日本のお客様は、ベイバイオサイエンスジャパンBay Biosciences Japanまたはhttp://baybiosciences-jp.com/contact/までご連絡ください。